FAQs
What is PRF?
PRF (Platelet-Rich Fibrin) is a concentrated blood product that contains a high concentration of platelets and fibrin. It is obtained from the patient’s own blood without the need for anticoagulants or additives. PRF is a natural product that has been used in various surgical procedures in dentistry, orthopedics, ophthalmology, and dermatology to promote wound healing and tissue regeneration.
During the centrifugation of a blood sample, a semi-solid clot called A-PRF (Advanced Platelet-Rich Fibrin) and a liquid called i-PRF (Injectable Platelet-Rich Fibrin) are obtained. These components are then used to accelerate the healing of bone and soft tissues in procedures such as periodontal surgeries, extractions, bone grafts, soft tissue grafts, and implant placement.
The advantages of PRF for patients include:
Being a 100% compatible product derived from their own blood.
Faster and higher-quality tissue regeneration.
Reduced inflammation and infections.
Less post-operative pain.
In our practice, PRF has various applications, including:
Placement of dental implants.
Substituting for a graft in certain gingival graft procedures.
Enhancing the healing of extraction sockets or bone graft sites.
Sinus bone grafting for dental implant placement in the maxillary sinus.
Overall, it is used in numerous surgical interventions to optimize the healing of soft (gum) and hard tissues (bone).
PRF offers significant benefits in periodontics and implantology, providing improved outcomes and enhanced healing for patients.
Is the laser new in dentistry?
Following its invention in the early 1960s, the laser was initially used experimentally on teeth and gums, and then in dentistry for gum treatment and oral surgery. In 1997, the FDA (Food and Drug Administration of the United States) approved the use of new lasers for the treatment of dental caries, a technology that the organization deemed “Medicine of the 21st century.”
Today, lasers are used worldwide by dentists to the great satisfaction of patients.
Which lasers do we use?
We use an Er,Cr:YSGG laser called “Waterlase iPlus,” which emits an invisible pulsed beam in the mid-infrared range of the electromagnetic spectrum.
We also utilize Diode lasers with various wavelengths in the visible and near-infrared spectra.
Is the laser safe?
In the hands of a competent and qualified dentist and hygienist, the laser is considered safe. Since it operates at low energy levels, it is suitable for treating delicate oral tissues. Furthermore, the controlled emission of heat and light from the laser helps eliminate virtually all bacteria and viruses from the treated site.
What is conventional periodontal therapy?
Usually, conventional therapy is performed in three or four phases:
A. Root Planing & Scaling
Conventional treatment aimed at cleaning the root surfaces and removing tartar. It may result in reattachment of the gum tissue, but not new attachment, leading to firmer tissue. However, the pockets may still persist. The periodontal status is reevaluated after a few weeks. If deep pockets persist, the next steps involve occlusal control and bone surgery.
B. Occlusal Control and Tooth Mobility
We also need to address excessive forces exerted on your teeth, which can contribute to instability at the treated site. First, we identify teeth that receive excessive force during chewing and check for habits such as grinding (bruxism) or clenching. These factors can hinder the desired outcomes. This part of the therapy aims to stabilize the occlusion. Three treatment modalities are used based on your needs: occlusal adjustment (selective grinding of teeth), splinting of mobile teeth, and wearing a nightguard to control bad habits. One or more of these modalities may be required depending on the case.
C. Bone Surgery
This surgery involves detaching and removing a portion of the gum tissue, root planing with reshaping and/or bone grafting, followed by closure of the gum with sutures. With bone grafting, new attachment can occur, and reattachment of the gum tissue is also possible. It may cause root hypersensitivity and tooth recession. After undergoing periodontal surgery, a portion of your gum tissue has generally been removed. If pockets redevelop, it is not always possible to repeat this procedure and remove more gum tissue indefinitely.
D. Maintenance of Oral Hygiene
Susceptibility to periodontitis persists throughout life, and regular hygiene recall visits (cleanings with a dental hygienist) are necessary regardless of the chosen treatment. It is a chronic disease that can be controlled but not cured. Additionally, it is transmissible but not contagious. This means that intimate and repeated exposure to periodontal bacteria can lead to infection in close contacts if they are susceptible to these bacteria.
How does laser therapy work?
Periodontal laser therapy (PLT) helps reduce pocket depth, thereby aiding in controlling and preventing the progression of periodontal disease. This procedure does not involve the removal of a portion of your gum tissue but aims to preserve as much tissue as possible so that it can reattach to your teeth.
The laser eliminates the inflamed inner portion of the gum without damaging the healthy part, providing better visibility for tartar removal. An ultrasonic device is then used to pulverize the tartar and irrigate the periodontal pocket. Conventional curettes can also be used to scale the root surfaces, and the laser’s biostimulatory effect may promote bone regeneration in certain cases.
This technique does not sterilize the periodontal pocket or permanently seal the gum to the tooth. Instead, it creates a favorable and more stable environment that allows the body to activate its own defense mechanisms. We tip the balance in favor of your immune system so that it can overcome the bacteria responsible for your gum infection. The laser also produces a photobiomodulation effect on the affected tissues. The deep-penetrating waves into the tissues, bone, and blood circulation act as anti-inflammatory and analgesic agents (biosuppression) and promote both bone and gum healing (biostimulation).
Once we have created a stable and disinfected environment through laser therapy, we also need to control excessive forces exerted on your teeth, which contribute to the instability of the treated site. We must identify the teeth that receive excessive force during chewing and check for habits such as grinding (bruxism) or clenching. These factors can hinder the achievement of desired results. This part of the therapy aims to stabilize the occlusion. Three treatment modalities are used based on your needs: occlusal adjustment (selective grinding of teeth), splinting of mobile teeth, and the use of a nightguard to control bad habits. One or more of these modalities may be required depending on the case.
After treatment, to avoid disturbing the treated site:
A surgical dressing will likely be applied to the treated area.
Once the dressing is removed or falls off, we will instruct you to start gently cleaning your teeth and avoid eating foods containing small particles, seeds, or pits for a few weeks.
Four to seven days after the procedure, we will schedule a follow-up appointment to remove the dressing and perform laser disinfection of the treated area.
You must follow the prescribed hygiene instructions and recall protocol.
Subsequently, to reassess and maintain the treated sites, we will need to see you for hygiene recall appointments every three months for one year. Three-month recall appointments are the best-known assurance to achieve optimal results in periodontics. Research shows that this fragile attachment that has just formed is susceptible to re-attack by periodontal bacteria. It takes about three months for these bacteria to organize and become detrimental to your oral health.
The advantages of laser therapy compared to conventional therapy are as follows:
• Less pain, swelling, bleeding, and post-operative infections.
• Reduced gum recession and therefore less post-operative sensitivity, particularly to hot, cold, and sugar.
• Shorter recovery period and less time off work.
• Overall, higher patient satisfaction rates.
Patients who have received laser treatments generally have a more positive experience during their dental visits and enjoy a more comfortable recovery in the days following the procedure.
Will I need local anesthesia when using the laser?
Yes, we recommend local anesthesia to ensure your comfort throughout the duration of your laser treatment.
What sensation will I experience during my laser treatment?
You will hear a dull popping sound and the sound of air blowing. Once the treatment begins, you will feel the pressure of the handpiece and a stream of water.
How to know if I am a good candidate for laser treatment?
Ask us! Following your examination and diagnosis, we are able to determine if laser treatment is a good option for you.
What are the stages of periodontal laser therapy?
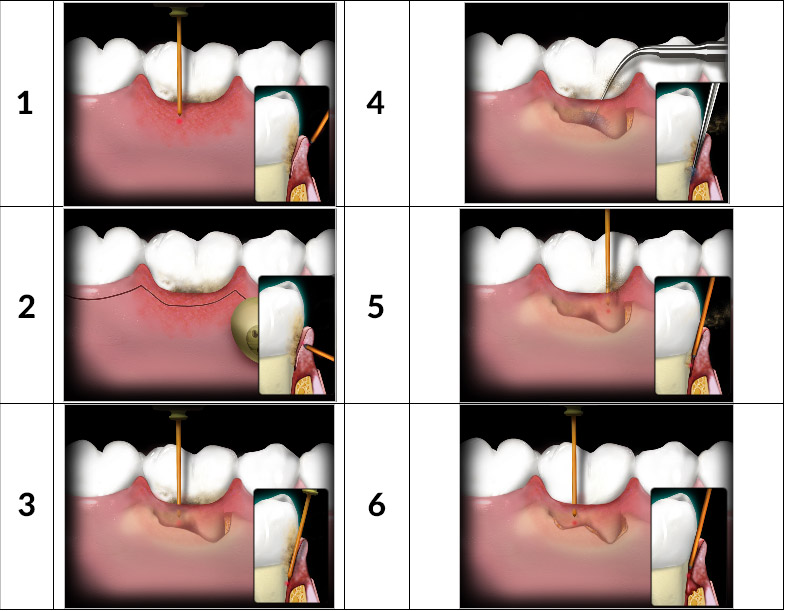
1. Removal of the outer soft tissue layer.
2. Remodelling of gingiva when too thick.
3. Removal of infected tissue inside the periodontal pocket.
4. Piezoelectric scaler and hand instruments are used to remove tartar deposits from the roots.
5. Final laser scaling with root disinfection.
6. Final laser debridement of the wound (formation of the blood clot that starts the healing chain).
Pour plus d’information générale sur les maladies parodontales et le rôle du parodontiste
Schedule An Appointment
Book online or call to schedule an appointment.
 Call Us
Call Us